Introduction
The importance of progesterone in hormone therapy
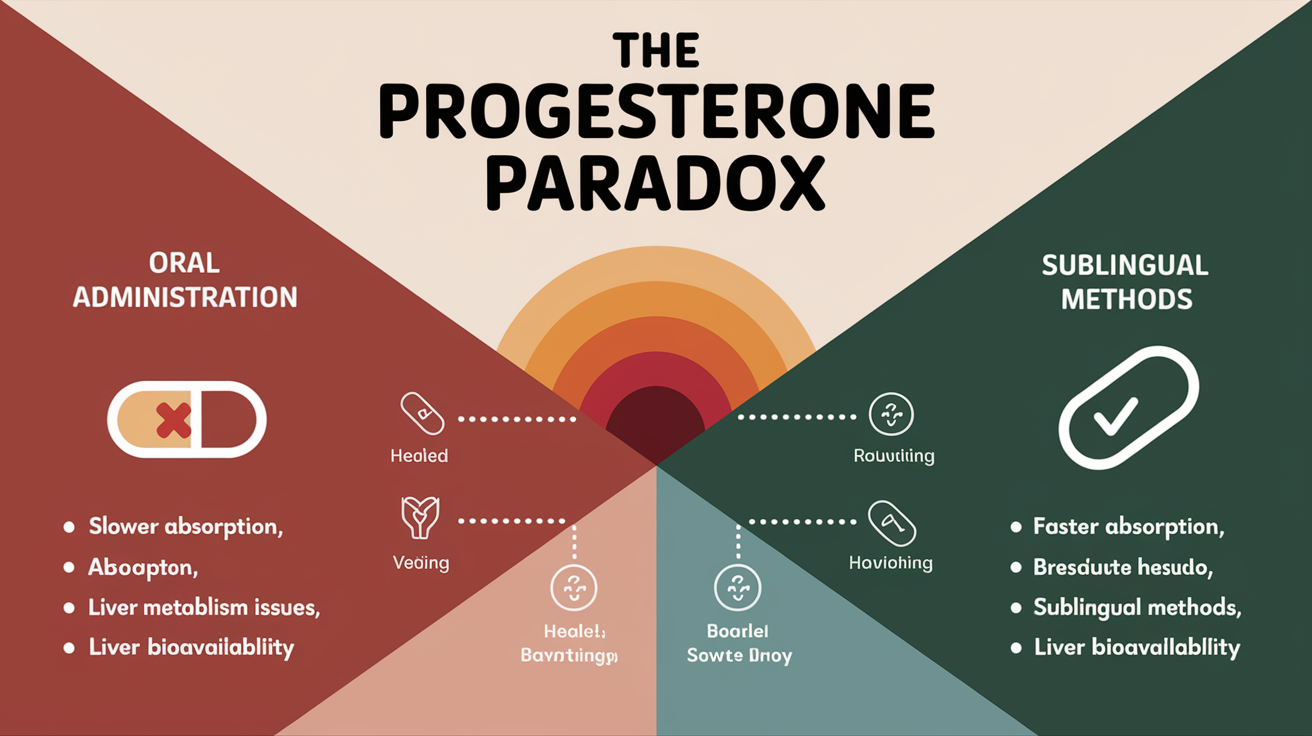
Progesterone is a crucial hormone, particularly in women's health, playing a vital role in the menstrual cycle, pregnancy, and overall hormonal balance. In hormone therapy, progesterone is often prescribed to counter the effects of estrogen, especially in postmenopausal women, to protect the endometrium from hyperplasia and potential cancer. It is also used to manage conditions like premenstrual syndrome (PMS), endometriosis, and to support fertility. The effectiveness of progesterone therapy, however, hinges significantly on the method of administration and its subsequent bioavailability.
Overview of administration methods
Progesterone can be administered through various routes, including oral pills, intramuscular injections, vaginal suppositories or creams, transdermal patches, and sublingual lozenges or drops. Each method presents different pharmacokinetic profiles, affecting how the hormone is absorbed, metabolized, and utilized by the body. Oral progesterone, the traditional approach, undergoes significant first-pass metabolism in the liver, reducing its bioavailability. Sublingual administration, on the other hand, bypasses this hepatic metabolism, potentially leading to higher and more consistent serum progesterone levels. This difference in absorption and metabolism is a key factor when considering the efficacy of different progesterone restoration strategies.
Background/Context
Progesterone's role in the body
Progesterone, a steroid hormone, is primarily secreted by the corpus luteum in the ovary during the second half of the menstrual cycle. Its primary function is to prepare the uterine lining for implantation of a fertilized egg and to maintain the pregnancy. Beyond its reproductive functions, progesterone affects various other systems in the body, including the brain, bones, and cardiovascular system. It has calming effects on the nervous system, supports bone density, and may influence mood and cognitive function. In the absence of pregnancy, progesterone levels decline, leading to menstruation. This cyclical rise and fall of progesterone are essential for maintaining hormonal equilibrium in women. Progesterone receptor signalling leads to down-regulation of estrogen receptors and restrains local estradiol production through interference with aromatase and 17 beta-hydroxysteroid dehydrogenase type 1 (Reis et al., 2020).
History of progesterone therapy
The use of progesterone in therapy dates back several decades, initially with synthetic progestins in oral contraceptives. Natural progesterone became available later, offering a bioidentical alternative for hormone replacement therapy (HRT). Early formulations primarily involved oral administration, but limitations in bioavailability led to the development of alternative routes. The Women's Health Initiative (WHI) studies significantly influenced the landscape of HRT, raising concerns about the risks associated with certain synthetic hormones and combination therapies (Farhat et al., 2013). This prompted a surge in interest in bioidentical hormone therapy, including natural progesterone, and alternative delivery methods like transdermal and sublingual routes (Bhavnani & Stanczyk, 2012).
Challenges in hormone restoration
Hormone restoration aims to alleviate symptoms associated with hormonal imbalances, such as those experienced during menopause or PMS. However, achieving optimal hormone levels can be challenging due to individual variations in absorption, metabolism, and receptor sensitivity. One of the main hurdles is delivering the hormone in a manner that mimics the body's natural production and maintains consistent levels without causing significant side effects. Oral administration often struggles with these challenges due to the first-pass effect, while other routes attempt to provide more direct and stable hormone delivery. Furthermore, the appropriate dosage and type of progestogen must be tailored to the individual's specific needs and health profile to minimize risks and maximize benefits.
Oral Progesterone: The Traditional Approach
How oral progesterone works
Oral progesterone is ingested and travels through the digestive system, where it is absorbed primarily in the small intestine. Once absorbed, it enters the portal vein and is transported directly to the liver. The liver then metabolizes a significant portion of the progesterone molecule before it can reach the systemic circulation. This metabolic process involves enzymatic breakdown, which reduces the amount of active progesterone available for use by the body. The remaining progesterone, along with its metabolites, then enters the bloodstream and is distributed to various tissues and organs.
Absorption and metabolism in the digestive system
The absorption of oral progesterone is influenced by several factors, including the formulation of the drug (e.g., micronized vs. non-micronized), the presence of food in the stomach, and individual differences in gastrointestinal function. Micronized progesterone, which consists of smaller particles, tends to be better absorbed than non-micronized forms. However, even with micronization, the absorption process is inherently variable. After absorption, the progesterone undergoes extensive first-pass metabolism in the liver, which significantly alters its chemical structure and reduces its concentration. This hepatic metabolism results in the production of various metabolites, some of which have their own biological activity, though typically weaker than that of progesterone itself.
Bioavailability issues
Bioavailability refers to the proportion of a drug that enters the circulation in an unchanged form and is available to exert its effect on the target tissues. Oral progesterone suffers from poor bioavailability due to the first-pass effect. Studies have shown that only a small percentage of the ingested progesterone actually reaches the systemic circulation in its active form. This low bioavailability necessitates higher doses to achieve therapeutic levels, which can increase the risk of side effects. The variability in absorption and metabolism further contributes to inconsistent hormone levels, making it difficult to achieve stable and predictable therapeutic outcomes.
First-pass metabolism effect
The first-pass metabolism effect is the primary reason for the low bioavailability of oral progesterone. When progesterone is absorbed from the gastrointestinal tract, it enters the hepatic portal system and is transported directly to the liver before entering the systemic circulation. The liver contains a variety of enzymes that metabolize drugs, including progesterone. These enzymes break down the progesterone molecule, reducing its concentration and converting it into inactive or less active metabolites. This process significantly diminishes the amount of progesterone available to exert its effects on target tissues, requiring higher oral doses to compensate for the loss. Bypassing this first-pass effect is a key advantage of alternative administration methods like sublingual delivery (Bassani et al., 2017).
Limitations of Oral Progesterone
Low absorption rates
The most significant limitation of oral progesterone is its low and inconsistent absorption rate. As discussed, the first-pass metabolism in the liver drastically reduces the amount of active progesterone that reaches the bloodstream. Studies have consistently demonstrated that oral progesterone has a significantly lower bioavailability compared to other routes of administration, such as vaginal or sublingual. This means that a larger dose is required to achieve the same therapeutic effect, which can increase the potential for side effects.
Inconsistent hormone levels
Due to variable absorption and metabolism, oral progesterone often leads to inconsistent hormone levels in the body. Factors such as individual differences in liver enzyme activity, gastrointestinal motility, and food intake can all affect how much progesterone is absorbed and metabolized. This variability makes it challenging to achieve stable and predictable hormone levels, which is crucial for effective symptom management. Fluctuating hormone levels can lead to breakthrough symptoms or side effects, reducing the overall effectiveness of the therapy.
Side effects and risks
While progesterone is generally considered safe, oral administration can be associated with certain side effects, particularly at higher doses required to compensate for low bioavailability. Common side effects include drowsiness, dizziness, mood changes, and gastrointestinal disturbances. Some women may also experience headaches, breast tenderness, or changes in libido. In addition, certain metabolites produced during the first-pass metabolism of oral progesterone may contribute to these side effects. While the slight decrease in serum progesterone levels with EPT therapy are uncertain, still there are potential treatment interactions for estrogenic hormones were identified, which suggest a larger response to HT in women with low endogenous levels (Edlefsen et al., 2010).
Inefficiency in symptom management
Because of low bioavailability and inconsistent hormone levels, oral progesterone may be less effective in managing symptoms compared to other delivery methods. For conditions like PMS, menopausal symptoms, or luteal phase defects, consistent and adequate progesterone levels are essential for symptom relief. The variability associated with oral progesterone can result in inadequate symptom control, leading to frustration and reduced quality of life for patients. This inefficiency often prompts healthcare providers to explore alternative routes of administration that offer more reliable hormone delivery.
Sublingual Administration: A Superior Alternative
Mechanism of sublingual delivery
Sublingual administration involves placing a progesterone lozenge or drops under the tongue, allowing the hormone to be absorbed directly into the bloodstream through the mucous membranes lining the floor of the mouth. This route bypasses the digestive system and the first-pass metabolism in the liver. The rich network of blood vessels under the tongue facilitates rapid absorption, allowing the progesterone to enter the systemic circulation quickly and efficiently. This direct entry leads to higher bioavailability and more consistent hormone levels compared to oral administration.
Types of sublingual progesterone
Lozenges
Sublingual lozenges are solid dosage forms designed to dissolve slowly under the tongue. They typically contain micronized progesterone mixed with inactive ingredients that aid in dissolution and absorption. Lozenges offer a convenient and relatively easy way to administer progesterone sublingually. Patients are instructed to place the lozenge under the tongue and allow it to dissolve completely without swallowing, which can reduce the amount of progesterone absorbed through the sublingual route.
Drops
Sublingual drops consist of a liquid formulation of progesterone that is administered under the tongue using a dropper. The liquid form allows for rapid dispersion and absorption through the oral mucosa. Some patients may find drops easier to administer than lozenges, especially if they have difficulty with dry mouth or swallowing. The dosage can also be easily adjusted by varying the number of drops administered. Like lozenges, patients are instructed to hold the drops under the tongue for a period of time to maximize absorption.
Advantages of sublingual administration
Sublingual administration offers several key advantages over oral progesterone. The most significant benefit is the avoidance of first-pass metabolism, which results in higher bioavailability and more consistent hormone levels. This can lead to more effective symptom management and a reduced risk of side effects. Sublingual delivery also offers a faster onset of action, as the progesterone enters the bloodstream more quickly compared to oral administration. Furthermore, sublingual formulations are generally well-tolerated and convenient to use, which can improve patient compliance.
Comparative Efficacy: Oral vs. Sublingual Progesterone
Absorption rates and bioavailability
The primary difference between oral and sublingual progesterone lies in their absorption rates and bioavailability. Oral progesterone is subject to significant first-pass metabolism, resulting in low and variable bioavailability, typically ranging from 1% to 10%. In contrast, sublingual progesterone bypasses the liver, leading to higher bioavailability, often reported to be in the range of 20% to 30% or even higher in some studies. This difference in bioavailability means that a lower dose of sublingual progesterone can achieve the same therapeutic effect as a higher dose of oral progesterone.
Hormone level stability
Sublingual progesterone tends to provide more stable hormone levels compared to oral administration. Because it bypasses the first-pass effect, the amount of progesterone entering the bloodstream is more predictable and consistent. This stability is crucial for maintaining a steady therapeutic effect and avoiding fluctuations that can lead to breakthrough symptoms or side effects. Oral progesterone, with its variable absorption and metabolism, is more likely to result in fluctuating hormone levels, making it more challenging to achieve optimal symptom control.
Symptom relief and management
Due to its superior bioavailability and hormone level stability, sublingual progesterone often provides more effective symptom relief and management compared to oral progesterone. Studies and clinical experience suggest that sublingual progesterone can be particularly beneficial for conditions like PMS, menopausal symptoms, and luteal phase defects, where consistent and adequate progesterone levels are essential. The improved symptom control can lead to a better quality of life for patients and increased satisfaction with the therapy.
Patient satisfaction and compliance
Patient satisfaction and compliance are often higher with sublingual progesterone compared to oral progesterone. The convenience of sublingual administration, combined with its improved efficacy and reduced side effects, can make it a more appealing option for many women. Patients are more likely to adhere to a treatment regimen that provides effective symptom relief and is easy to use. The faster onset of action with sublingual delivery can also contribute to increased patient satisfaction, as they experience symptom relief more quickly.
The Science Behind Sublingual Superiority
Pharmacokinetics of sublingual progesterone
The pharmacokinetics of sublingual progesterone differ significantly from that of oral progesterone. After sublingual administration, progesterone is rapidly absorbed through the oral mucosa and enters the systemic circulation directly. This rapid absorption results in a faster onset of action and higher peak plasma concentrations compared to oral administration. The absorption rate can be influenced by factors such as the formulation of the drug, the amount of saliva in the mouth, and the duration of contact with the sublingual mucosa.
Bypassing hepatic first-pass metabolism
The key to sublingual progesterone's superiority lies in its ability to bypass hepatic first-pass metabolism. By avoiding the liver, the progesterone molecule remains intact and is not broken down into inactive or less active metabolites. This results in a significantly higher proportion of the administered dose reaching the target tissues in its active form. This is in stark contrast to oral progesterone, where a large percentage of the drug is metabolized in the liver before it can exert its effects.
Direct entry into systemic circulation
The direct entry of sublingual progesterone into the systemic circulation has several important implications. First, it allows for more predictable and consistent hormone levels, as the absorption process is less susceptible to individual variations in gastrointestinal function and liver enzyme activity. Second, it reduces the risk of side effects associated with progesterone metabolites produced during first-pass metabolism. Third, it allows for a lower dose to achieve the same therapeutic effect as a higher dose of oral progesterone.
Tissue-specific effects
While progesterone exerts its effects on various tissues throughout the body, its primary target is the uterus, where it prepares the endometrium for implantation. Sublingual progesterone, with its higher bioavailability and more consistent hormone levels, can more effectively target the uterus and exert its desired effects. This is particularly important for women undergoing fertility treatments or those at risk of endometrial hyperplasia. The ability to achieve adequate progesterone levels in the uterus is crucial for successful outcomes in these situations.
Clinical Evidence and Research Findings
Studies comparing oral and sublingual progesterone
Several studies have compared the efficacy of oral and sublingual progesterone. These studies consistently demonstrate that sublingual progesterone has higher bioavailability and results in more stable hormone levels compared to oral progesterone. For example, research has shown that sublingual micronized progesterone achieves significantly higher serum progesterone concentrations than oral micronized progesterone at the same dose. Furthermore, studies have indicated better perinatal perspectives in patients treated with combination therapy of preterm labor with the sublingual form of vaginal micronized progesterone compared with pregnant women who received oily solution progesterone i.m (Голяновський et al., 2016). These findings support the use of sublingual progesterone as a superior alternative to oral progesterone for hormone restoration.
Patient outcomes and experiences
Patient outcomes and experiences often reflect the superior pharmacokinetics of sublingual progesterone. Women who switch from oral progesterone to sublingual progesterone frequently report improved symptom control, reduced side effects, and increased satisfaction with their treatment. Many patients find the sublingual route more convenient and easier to adhere to compared to oral administration. These positive experiences contribute to improved compliance and better overall outcomes.
Expert opinions and recommendations
Many experts in the field of hormone therapy now recommend sublingual progesterone as a preferred alternative to oral progesterone. They cite the superior bioavailability, hormone level stability, and patient outcomes as reasons for their recommendation. Some experts also suggest that sublingual progesterone may be a safer option due to the reduced risk of side effects associated with first-pass metabolism. These expert opinions are based on a growing body of scientific evidence and clinical experience.
Analysis/Implications
Shifting paradigms in hormone therapy
The growing recognition of the limitations of oral progesterone and the advantages of sublingual administration is leading to a shift in paradigms in hormone therapy. Healthcare providers are increasingly adopting sublingual progesterone as a first-line treatment option for women with hormonal imbalances. This shift reflects a greater emphasis on individualized treatment approaches that take into account the unique pharmacokinetic properties of different hormone delivery methods. The relevance of the discussion about therapeutic and preventive effects of combined oral contraceptives is caused to the fact that their impact is quite often the primary motivation for the appointment and intake the drugs (Сергиенко et al., 2016).
Potential for improved treatment outcomes
The adoption of sublingual progesterone has the potential to significantly improve treatment outcomes for women with hormonal imbalances. By providing more stable and consistent hormone levels, sublingual progesterone can lead to better symptom control, reduced side effects, and increased patient satisfaction. This can translate into improved quality of life and a greater sense of well-being for women undergoing hormone therapy. The lower prevalence of headache and improved pattern of flushing and nasal congestion with sublingual Sild ODF suggests a possible implication also in the clinical efficacy profile (De Toni et al., 2018).
Challenges in adopting sublingual methods
Despite the clear advantages of sublingual progesterone, there are some challenges in adopting this method more widely. One challenge is the lack of awareness among healthcare providers and patients about the benefits of sublingual administration. Another challenge is the availability of sublingual progesterone formulations, which may be limited in some areas. Furthermore, some patients may find the taste or texture of sublingual lozenges or drops unpleasant, which can affect compliance. Overcoming these challenges requires education, increased availability of sublingual formulations, and development of more palatable products.
Conclusion
Recap of key points
In summary, oral progesterone is a very ineffective hormone restoration strategy compared to sublingual lozenges or drops due to its low bioavailability, inconsistent hormone levels, and potential for side effects associated with first-pass metabolism. Sublingual administration bypasses the liver, resulting in higher bioavailability, more stable hormone levels, and improved symptom control. Clinical evidence and expert opinions support the use of sublingual progesterone as a superior alternative to oral progesterone for hormone therapy.
Future directions in progesterone therapy
Future research in progesterone therapy should focus on optimizing sublingual formulations to improve taste, texture, and absorption. Studies are needed to further compare the efficacy of sublingual progesterone with other routes of administration, such as vaginal and transdermal. Additional research is also needed to investigate the long-term effects of sublingual progesterone on various health outcomes.
Call to action for healthcare providers and patients
Healthcare providers are encouraged to consider sublingual progesterone as a first-line treatment option for women with hormonal imbalances. They should educate themselves and their patients about the benefits of sublingual administration and ensure that appropriate formulations are available. Patients should discuss their hormone therapy options with their healthcare providers and consider whether sublingual progesterone may be a better choice for them. By working together, healthcare providers and patients can optimize hormone therapy and improve the health and well-being of women.
REFERENCES:
Reis, F. M., Coutinho, L. M., Vannuccini, S., Batteux, F., Chapron, C., & Petraglia, F. (2020). Progesterone receptor ligands for the treatment of endometriosis: the mechanisms behind therapeutic success and failure. In Human Reproduction Update (Vol. 26, Issue 4, pp. 565–585). Oxford University Press (OUP). https://doi.org/10.1093/humupd/dmaa009
Farhat, G. N., Parimi, N., Chlebowski, R. T., Manson, J. E., Anderson, G., Huang, A. J., Vittinghoff, E., Lee, J. S., LaCroix, A. Z., Cauley, J. A., Jackson, R., Grady, D., Lane, D. S., Phillips, L., Simon, M. S., & Cummings, S. R. (2013). Sex Hormone Levels and Risk of Breast Cancer With Estrogen Plus Progestin. In JNCI Journal of the National Cancer Institute (Vol. 105, Issue 19, pp. 1496–1503). Oxford University Press (OUP). https://doi.org/10.1093/jnci/djt243
Bhavnani, B. R., & Stanczyk, F. Z. (2012). Misconception and Concerns about Bioidentical Hormones Used for Custom-Compounded Hormone Therapy. In The Journal of Clinical Endocrinology & Metabolism (Vol. 97, Issue 3, pp. 756–759). The Endocrine Society. https://doi.org/10.1210/jc.2011-2492
Bassani, A. S., Banov, D., & Carvalho, M. (2017). Evaluation of the in vitro Human Skin Percutaneous Absorption of Progesterone in Versabase® Using the Franz Skin Finite Dose Model. In Journal of Womens Health Care (Vol. 06, Issue 04). OMICS Publishing Group. https://doi.org/10.4172/2167-0420.1000384
Edlefsen, K. L., Jackson, R. D., Prentice, R. L., Janssen, I., Rajkovic, A., O’Sullivan, M. J., & Anderson, G. (2010). The effects of postmenopausal hormone therapy on serum estrogen, progesterone, and sex hormone-binding globulin levels in healthy postmenopausal women. In Menopause (Vol. 17, Issue 3, pp. 622–629). Ovid Technologies (Wolters Kluwer Health). https://doi.org/10.1097/gme.0b013e3181cb49e9
Голяновський, О. В., Рубінштейн, А. М., & Бачинська, М. А. (2016). The effectiveness of micronized progesterone sublingual and vaginal forms combined use in the treatment of preterm labor. In Reproductive Endocrinology (Vol. 0, Issue 27, p. 41). Publishing Office TRILIST. https://doi.org/10.18370/2309-4117.2016.27.41-46
Сергиенко, М. Ю., Сюсюка, В. Г., & Колокот, Н. Г. (2016). Creativity and individuality in matters of hormonal contraception. In Reproductive Endocrinology (Vol. 0, Issue 31, pp. 54–59). Publishing Office TRILIST. https://doi.org/10.18370/2309-4117.2016.31.54-59
DOI
De Toni, L., De Rocco Ponce, M., Franceschinis, E., Dall’Acqua, S., Padrini, R., Realdon, N., Garolla, A., & Foresta, C. (2018). Sublingual Administration of Sildenafil Oro-dispersible Film: New Profiles of Drug Tolerability and Pharmacokinetics for PDE5 Inhibitors. In Frontiers in Pharmacology (Vol. 9). Frontiers Media SA. https://doi.org/10.3389/fphar.2018.00059