Gentle, Real Tips from One Mom to Another
If you’re here, you’re likely struggling with latching. I’ve been there — crying in the middle of the night, wondering if I’m doing this “mom thing” wrong. You’re not alone. Every mom I know has faced this frustration at least once. So let’s talk, not as experts, but as moms sharing what works.
First, What Is a “Good” Latch?
A good latch means:
Baby’s mouth covers not just the nipple, but a wide portion of the areola (the darker skin around it).
You feel a tugging sensation, not sharp pain.
Baby’s chin presses into your breast, with lips flanged out like a fish’s.
You hear steady sucking and swallowing sounds.
It doesn’t have to be perfect. A good latch is one that feels okay for you and lets your baby feed effectively. That’s enough.
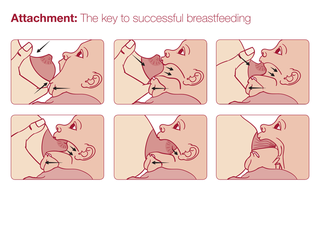

Wide mouth: Baby’s mouth is open at a 120–140° angle, like a big yawn.
Flanged lips: Top and bottom lips are curled outward, not tucked in.
Chin pressed in: Baby’s chin touches the breast, nose lightly grazes or stays clear.
No cheek dimpling: Cheeks are rounded, not sucked in.
Areola coverage: Most of the areola (especially the bottom part) is in the mouth. Include labels pointing to these features and a small “X” showing incorrect latch (tucked lips, shallow grip).
Why Is Latching So Hard?
Latching issues can come from:
Flat or inverted nipples.
Engorgement (breasts too full).
Baby’s tiny mouth or weak muscle tone (common in newborns or preemies).
Birth challenges (c-section, NICU stay, tongue or lip tie).
Awkward positioning or lack of support.
Here’s the truth nobody says: It’s not always your fault. Our bodies and babies are unique, and the system expects moms to figure this out on no sleep and little guidance. That’s not fair.
For Moms in Specific Situations:
Working moms: Pumping between feeds can help maintain supply if you’re away from baby.
NICU or preemie moms: Kangaroo care (skin-to-skin) can encourage latching instincts even before full feeds.
Cultural considerations: If your family has specific breastfeeding traditions, blend them with these tips or ask a lactation consultant to adapt them.
Step-by-Step: The Gentle Latch Method That Works
Get comfortable. Use a supportive chair, pillows behind your back, and one under your arm. If you’re tense, baby senses it.
Tummy to tummy. Position baby so their belly faces yours. Bring baby to your breast, not your breast to baby.
Nose-to-nipple alignment. Hold baby so their nose is level with your nipple. This encourages a head tilt and wide mouth.
Wait for a wide mouth. Tickle baby’s upper lip with your nipple until they open wide, like a yawn. Be patient!
Quick, firm pull-in. Smoothly bring baby onto the breast, guiding from the shoulders or neck, not pushing the head.
Check the signs:
Lips flanged out (like a fish).
Chin pressed deeply into the breast.
Tugging sensation, not pain.
Steady sucking and swallowing sounds.
Visual Tip: If baby’s cheeks dimple or you hear clicking noises, the latch is too shallow. Gently unlatch and try again.
Troubleshooting: If It Hurts
Break the seal. Slide a clean pinky into the corner of baby’s mouth to stop suction, then unlatch. Try again with a wider mouth.
Check for tongue or lip tie. Persistent pain, poor weight gain, or clicking sounds may suggest a tie. Ask a pediatrician or IBCLC (International Board Certified Lactation Consultant) for an evaluation. Ties are fixable with minor procedures.
Try different positions:
:max_bytes(150000):strip_icc()/common-breastfeeding-positions-431648_final-73bc9a2330874843b4d7e2650220b6ec.png)
Football hold: Baby tucked under your arm, great for c-section recovery or small babies.
Side-lying: Lie on your side with baby facing you, perfect for night feeds or tired moms.
Laid-back (biological nurturing): Recline slightly, let baby lie on your chest, ideal for overactive letdown.
When to Seek Help: If pain lasts beyond the first minute of feeding, or you notice cracked nipples, bleeding, or no improvement after a week, contact an IBCLC. Find one at ILCA.org or ask your hospital.
What If It’s Not the Latch? Common Pain Causes
Pain isn’t always about latching. Here’s what to look for:
Nipple thrush (yeast infection): Burning, stabbing pain during or between feeds, sometimes with white patches in baby’s mouth. Treatment: Antifungal cream (prescribed by a doctor) and sterilizing pump parts.
Vasospasms (Raynaud’s phenomenon): Nipples turn white, red, or blue after feeds with sharp, burning pain. Keep breasts warm and consult a doctor for possible medication.
Dermatitis or eczema: Red, itchy, or flaky areola skin. Use hypoallergenic creams and avoid scented soaps. A doctor may suggest a mild steroid cream.
Self-Check Tip: After feeding, gently press your nipple. If it’s misshapen (like a lipstick tip), the latch needs adjusting. A round nipple means baby latched well.
What Helped Me Most (Real Mom Hacks)
Silver nipple cups: Naturally antibacterial, they soothe sore nipples between feeds.
Warm compresses: Apply before nursing to soften engorged breasts.
Hand-express a little milk: This softens the areola, making it easier for baby to latch.
Skin-to-skin time: Hold baby against your chest to calm them and trigger latching instincts.
Breastfeeding-safe lanolin or organic nipple balm: Apply after feeds to heal cracks.
Pumping for relief: If engorgement is severe, pump just enough to soften breasts.
Pro Tip for Working Moms: Store pumped milk in 2–4 oz portions for easier feeding later. Use a hands-free pump to save time.
Mental Health Matters: Coping with the Hard Days
Breastfeeding can feel overwhelming, especially if you’re battling pain, exhaustion, or self-doubt. Here’s what helped me:
Take micro-breaks. Even 5 minutes of deep breathing or a warm shower can reset you.
Ask for help. Tell your partner, friend, or family exactly what you need: a meal, a nap, or just someone to listen.
Connect with other moms. Join a local La Leche League group (LLLI.org) or online forums like KellyMom.
Watch for postpartum depression. If you feel hopeless or disconnected for more than a few days, talk to your doctor or call the PSI Helpline (1-800-944-4773).
Affirmation for You: “I’m learning with my baby. My effort is enough. We’re in this together.”
Resources to Support You
La Leche League (LLLI.org): Free breastfeeding support groups and hotlines.
KellyMom (KellyMom.com): Evidence-based breastfeeding info.
WIC Breastfeeding Support (signupwic.com/breastfeeding): Free resources for eligible moms in the US.
Postpartum Support International (Postpartum.net): Mental health support for new moms.
Find an IBCLC: Search at ILCA.org or ask your pediatrician.
Hotline for Immediate Help: Call the National Breastfeeding Helpline at 1-800-994-9662 (available in English and Spanish).
Final Thoughts from One Mom to Another
You are not failing. You and your baby are learning together, and that’s okay. Some days, it’ll click. Other days, you’ll need a deep breath and a retry.
If you’re a working mom, a preemie mom, or navigating cultural traditions, know that your journey is valid. Reach out for support — a lactation consultant, a friend, or even an online community. You deserve help, rest, and kindness.
Your love is already nourishing your baby. The milk will follow, and so will your rhythm.
But,milk isn’t jnly just in your breasts. It’s in your mind.
If you’re exhausted, doubting yourself, or Googling at 3AM…
This mini guide will give you peace, perspective, and the exact tracker that saved my sanity.
You’ll thank me later — tap below to download now.