Training Low
Traditionally, athletes have been recommended high carbohydrate diets during training periods. The theory being that by eating carbohydrates, glycogen stores are fully replenished and thus able to be used for energy.
Training low refers to training with low carbohydrate availability. There are many ways to achieve this, from consuming a low-carbohydrate diet and fasting to training multiple times a day to deplete glycogen stores.
There has not been a great deal of studies comparing a high-carb-low-fat (HCLF) vs low-carb-high-fat (LCHF) approach when it comes to exercising. But my understanding is that for high intensity exercises, high-carbohydrate diets are king. This is because the body is able to metabolise carbohydrates a lot quicker than fat.
However, theory dictates that a LCHF approach may be beneficial for endurance athletes to alter the type of fuel they rely on when training. The idea is that a LCHF approach helps the athlete easily tap into near-limitless stores of fat rather than their limited carbohydrate stores. This would allow athletes to go much further without ‘hitting the wall’ when carbohydrate stores become depleted.
It has been shown that athletes training low increase their ability to utilize fat as fuel. Conversely, those training with high carbohydrates seems to blunt expression of genes involved in fatty-acid metabolism rather than stimulate those involved in carbohydrate metabolism.
Unfortunately for endurance at lower intensity exercises such as cycling at 60% of VO2 max, current evidence concludes that low-carb high fat diets either have a small, positive effect, or no effect at all.
But this isn’t the whole story.
(This is a great article more about this topic with references - https://www.trainingpeaks.com/blog/low-vs-high-carbohydrate-diet-endurance/)
Why do I train low?
Over the last month I have run fasted (>16hr without food or supplements) over long distances. My longest being 20 miles.
I am not an athlete and not worried about fat loss. So why do I do this?
Two words.
Mitochondrial biogenesis.
From here on out I will be summarising an interesting study called -
Two of the many things this multi-armed study looked at were:
- The effect of exercise with low glycogen levels on markers of mitochondrial biogenesis.
- The acute effect of exercise on starvation-induced insulin resistance.
Conclusions regarding the subjects above are detailed below:
Training with low glycogen levels enhanced the response in markers of mitochondrial biogenesis.
Starvation-induced insulin resistance is attenuated by exercise. Mitochondrial respiration and reactive oxygen species (ROS) production is reduced during starvation. Exercise during starvation reduced glycogen stores and resulted in the activation of enzymes involved in glucose metabolism.
When exercise was performed during starvation there was an increase in markers for mitochondrial lipid oxidation.
I train fasted to:
- Enhance mitochondrial health and density.
- Attenuate starvation-induced insulin resistance.
- Increase mitochondrial lipid oxidation.
- Increase supportive reactive oxygen species.
If you would like to stop reading here you can, but if you would like to know more about the said things mentioned above – keep on reading – I have summarised points from the study above that I have found interesting. (See original study for references).
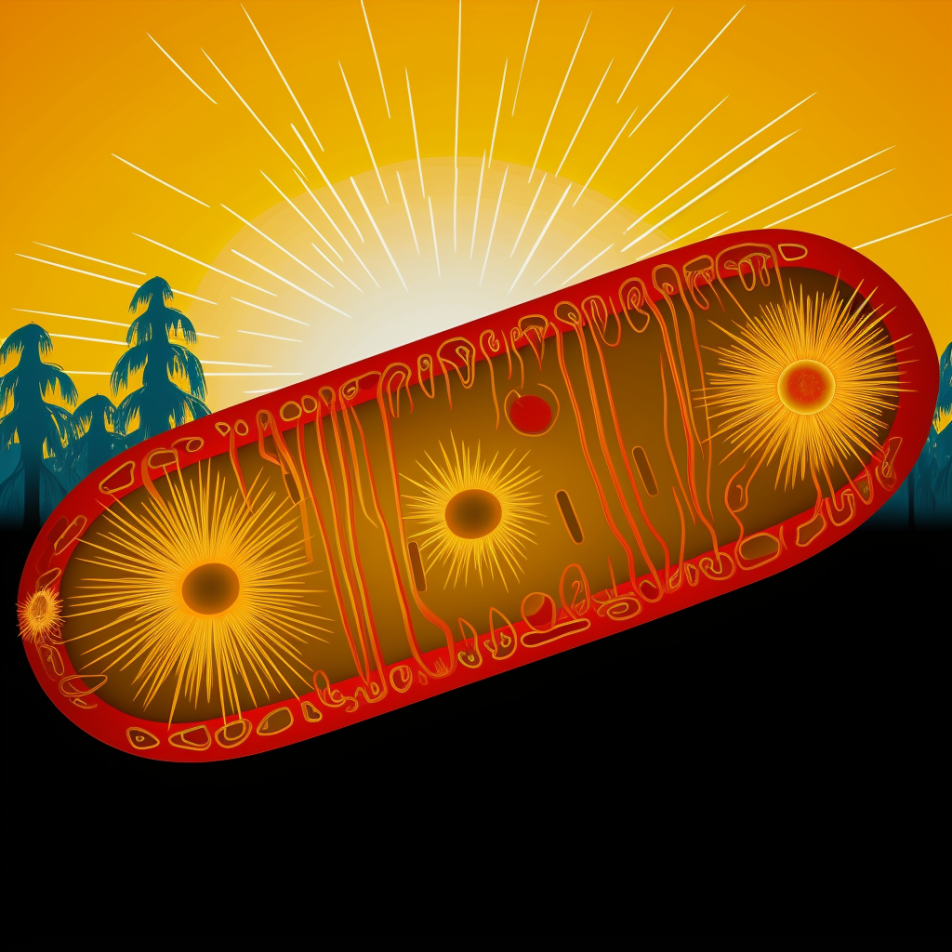
Mitochondria – Producer of energy and much more
Mitochondria are the powerhouse of the cell and its density and function have been associated with cardiovascular disease, insulin resistance and T2D, aging and aerobic capacity. Mitochondria transform energy from nutrients into adenosine triphosphate (ATP) via a process called oxidative phosphorylation.
Mitochondria also produce reactive oxygen species (ROS) as a by-product of oxidative phosphorylation. ROS are highly reactive molecules with the potential to damage cell structures – and thus have been viewed as something negative over the past few decades, however, more recently, this paper suggest that research has identified ROS as a regulator of cell signalling, which suggests a more complex role.
ROS production in mitochondria:
- Is increased in state 4 (basal) respiration compared to active state 3 (maximal ADP stimulated) respiration.
- Seems to be supportive when exercising – the suppression of ROS by antioxidant supplementation seems to blunt the response to exercise training.
- Is harmful when chronically elevated levels, while short intense exposure, e.g. following exercise, seems to activate cell signals.
PGC-1α – The mitochondrial growth serum
Peroxisome proliferator-activated receptor gamma coactivator 1-alpha (PGC-1α) is the master regulator of mitochondrial biogenesis. PGC-1α is also the primary regulator of liver gluconeogenesis, inducing increased gene expression for gluconeogenesis.
PGC-1α is a major regulator of mitochondrial biogenesis and plays an important role in cell metabolism. Exercise is a potent up-regulator of PGC-1α. Intracellular energy stress is another activator.
PGC1α activation seems also to be sensitive to the redox environment. Exposure of cultured myotubes with ROS caused an induction of PGC-1α. This is possibly why exercise also increases PGC1α.
The study concludes when training low – it is in fact the (low) glycogen content during exercise, rather than calorie intake, plasma insulin or fatty-acid levels, that is responsible for the pronounced increase in PGC-1α.
PGC-1α may also play a role in insulin sensitivity. PGC-1α gene expression is reduced in diabetics and this has led to the assumption that PGC-1α may be important for insulin sensitivity.
However very interestingly, genetically engineered mice contradict this hypothesis. When PGC-1α is over expressed, high-fat diet induced insulin resistance actually worsens. In contrast, exercising seems to be more insulin sensitizing in these mice compared to wild type mice.
Starvation and insulin resistance
Short-term starvation in humans induces insulin resistance. Within 24 hours of starvation, liver glycogen is depleted and thereafter insulin resistance develops in peripheral tissues.
The reduction in insulin sensitivity is an important physiological response to make sure glucose gets to the central nervous system.
There is a real danger of a hypoglycaemic event occurring whilst exercising fasted if one is not appropriately trained.
Thus, I would not advise fasted training without being fat-adapted and a having full knowledge of one physiology. Also consult a doctor beforehand.
In those who are fat adapted though, hypoglycaemia may not occur or be felt as starvation is associated with increased lipolysis, and increases in plasma fatty-acids and intramuscular triglycerides. Ketone production is also increased and used as fuel.
Exercise and insulin resistance
Skeletal muscle accounts for approximately 80% of glucose disposal, which makes the muscle tissue a major player for regulating blood glucose levels.
The first stage of developing T2D involves a reduced ability of muscular tissue to increase glucose uptake in response to insulin. To maintain blood glucose homeostasis, the body responds by increasing insulin secretion from pancreatic beta cells.
Increased lipolysis, plasma fatty-acids or intramyocellular triglycerides (IMTG) are common features of many conditions associated with reduced insulin sensitivity, e.g. obesity, T2D, lipid infusion, high-fat diet, and starvation. One theory suggests that an accumulation of IMTG causes insulin resistance.
Interestingly athletes as well as obese individuals have high IMTG levels – this is termed “the athlete’s paradox”. Current thinking is that in athletes, improved efficiency of trained skeletal muscles prevents the development of insulin resistance.
Mitochondrial dysfunction and Diabetes
In addition to having an increased level of IMTG, several studies show that individuals with insulin resistance or T2D have reduced mitochondrial content and function.
Based on these observations it has been suggested that inherited or acquired mitochondrial dysfunction compromises the ability to oxidize fat.
Mitochondrial dysfunction develops during diabetes and probably not because of it. When comparing healthy controls, pre-diabetics and longstanding T2D individuals, mitochondrial dysfunction was only found in the latter.
Conclusion
All-in-all I train fasted to improve my mitochondrial health. I believe that it was probably not uncommon for our hunter gathering ancestors to have hunted whilst hungry and therefore not ‘unnatural’. I may not be able to perform at peak levels whilst performing high intensity exercises but with fasted low intensity training I may be helping my body in more ways than one.
I do train not fasted all the time and believe in metabolic and physical training flexibility. Long term studies have not been performed in this area as of yet - but I believe training low over longer periods may maximise mitochondrial function and thus aid in overall function when training not fasted.
Furthermore, if nothing else it provides another way to fight chronic health conditions. Like with anything else, please take caution and seek medical advice beforehand. Hydrate well after training with added electrolytes and I recommend consuming high amounts of protein to stop/reduce muscle breakdown.
(This is not medical advice btw)
Interesting points:
Mitochondria produce ROS however the nature of the ROS is dependent on how and when it is made – at rest or exercise/acute or chronic.
ROS is not just harmful waste and may contribute to cell signalling.
When PGC-1α is over-expressed (in mice), high-fat diet-induced insulin resistance actually worsens.
Short-term starvation in humans induces insulin resistance.
Interestingly athletes as well as obese individuals have high IMTG levels – this is termed “the athlete’s paradox”.
Mitochondrial dysfunction develops during diabetes and exercise may help reverse it.